Our Nursing Team
At AMVS we have one of the largest veterinary nursing team in the south. The team consists of Registered Veterinary Nurses (RVNs), Student Veterinary Nurses (SVNs), Patient Care Assistants (PCAs) and Technicians, each working together across all of our disciplines and supporting the veterinary surgeons to provide the best care for the pets that are referred to us.
As a referral veterinary nurse you get to develop your skills in each of the disciplines that we offer from Neurology and Orthopaedics to Cardiology and Anaesthesia. The role is extremely varied you could be working on wards, in theatre or helping with imaging.
The duties of a qualified Veterinary Nurse involve a considerable amount of responsibility, such as monitoring anaesthesia, laboratory tests, phlebotomy, inpatient care and treatment, surgical assistant, infection control and much more. Senior nurses play a key role in the running of the practice.
Nurse profiles
Meet some of our team here and learn about how they got into veterinary nursing, as well as how we support them with continued professional development:
Katy is a Registered Veterinary Nurse (RVN) in our Internal Medicine team.
She shares the story of her career so far;
"I started as a student nurse in 2004 at a busy mixed animal hospital in the New Forest. I did my apprenticeship for nurse training and qualified in January 2007. I worked at the practice for ten years working with small and large animals. During this time I completed a graduate diploma in professional and clinical veterinary nursing and a certificate in feline friendly nursing.
In June 2014 I moved to Anderson Moores Veterinary Specialists where I have worked in a variety of departments. I started out as a multidisciplinary nurse which covered a rotation around each department within the hospital. I then moved to be a neurology nurse for a year before moving to the out of hours team and a night nurse for about three years. Following this I returned to the multidisciplinary department before landing my ideal job in the internal medicine department.
I really enjoy the variety of cases that we see in the medicine department"


Leila is a registered veterinary nurse (RVN) with an ISFM Certificate in Feline Nursing (CertFN), has completed a High-Risk Anaesthesia Course, VetsNow Certificate in Emergency and Critical Care, been a clinical coach ad Deputy Head Nurse and is now a Senior Wards Nurse and Wards Lead.
She shares the story of her career so far;
“I didn't know what I wanted to do when I left school, so ended up working in retail, then at 23 decided to go travelling. I had always wanted to work with animals so on my round the world trip, I volunteered at an animal adoption centre in Chicago called PAWS (the role was similar to a Patient Care Assistant). I took the dogs out every day and loved it! This made me want to pursue a career with animals. When I got back I volunteered at the RSPCA clinic in Southampton and wrote to all the veterinary practices in my area to ask for a student nurse position. I only had one reply and that was for a weekend receptionist position, but it gave me the foot in the door and soon became full-time!
“After a year they gave me an apprentice student nurse position. I went to college one day a week and worked as a full-time student nurse. After 3 years of training, I qualified as a Registered Veterinary Nurse. Then my career took off and I have undertaken lots of further qualifications and was a clinical coach and deputy Head Nurse.
“After 7 years in primary care, I decided to move into referral nursing to develop my skills further. I started at Anderson Moores in July 2019 as a multi-disciplinary nurse, which involves rotating through all the departments. My favourite departments to work in are Wards and Surgery. I have now become a Senior Wards nurse and Wards Lead.
“The team at Anderson Moores are fantastic! I enjoy working here because the patients get the very best care. I have learnt so much since starting, and they have supported my career development and ongoing professional development. I now have an incredibly exciting sabbatical opportunity later this year working at a hospital within the group based in Singapore!”


Read some of the day (and night) of the life experiences of our nurses
Here is a day in the life of one of our team leaders: Abi Jones, Wards Team Leader. DipAVN(Surg) CertVNECC RVN
With a nursing team of around 100 individuals including Patient Care Assistants, Technicians and the night team, the Nursing Team Leaders have a busy role in a specific area in the hospital with a number of key responsibilities.
Abi describes her day “I am Wards Team Leader and start the day with a brief huddle with the Senior Wards Nurse. This RVN (Registered Veterinary Nurse) has taken the handover from the night nurses, and will then attend rounds with the clinicians, starting with Medicine then Surgery working the way through all the patients finishing with Neurology. The Senior Wards Nurse allocates nurses to patients within our five wards, we try to keep the same nurses with the patients for the week as this allows a better patient nurse bonding.
There are four senior wards nurses who run wards on a rotation, I join in to cover holidays, but mostly I am nursing my own patients in the wards. I don’t have a favourite area, but I do find an enormous amount of job satisfaction when I am nursing in the high dependency unit, this is a small ward that allows monitoring of the sickest patients. In the last month I have nursed a patient with tetanus who had a tracheostomy tube and a patient who was being supported on a mechanical ventilator. As well as the high dependency unit we have two main dog wards an isolation ward and a separate cat ward.
While the Senior Wards Nurse is at rounds we can begin our first checks on the patients under our care. During our shift we unwrap the bandages and inspect the intravenous catheters on every patient. We inspect any surgical wounds, checking any indwelling devices inserted into the patient. There are a number of devices this could be, but some examples include a chest drain that allows the removal of accumulated air in a patient with a pneumothorax. Or a urinary catheter that we use to drain the bladder and collect urine to measure in a patient with an acute kidney injury (that could have been caused by Cutaneous and Renal Glomerular Vasculopathy (CRGV or Alabama rot). Or an Oesophagostomy feeding tube that allows us to provide nutrition to a patient who is unable to eat orally, for example a patient with an injured face following a road traffic accident.
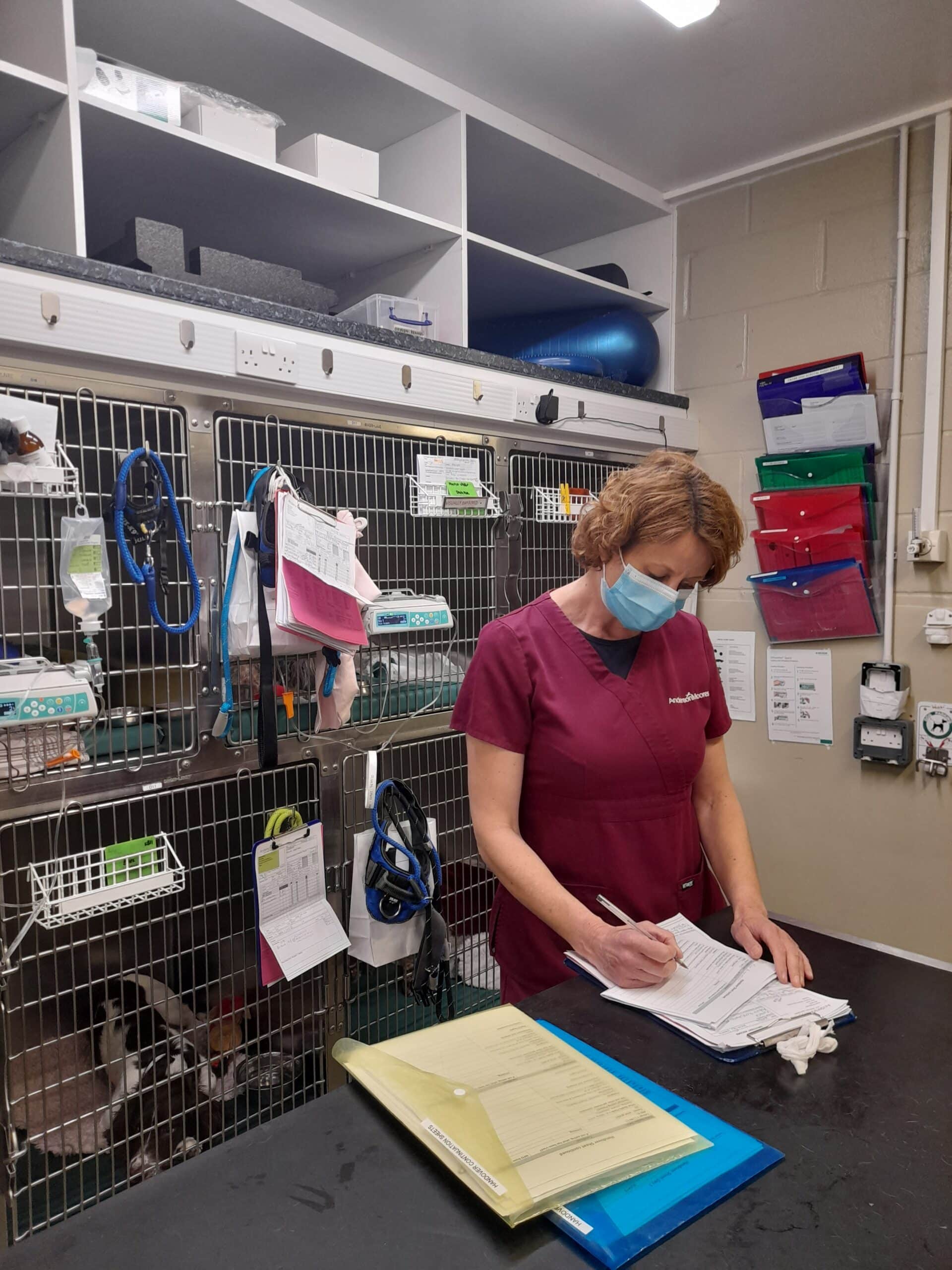
In this photo I am receiving a handover from the Surgical Nurse James, on my patient who has returned to the main dog ward following surgery to remove a cancerous lump from her leg and remove the local lymph node.
Our job is always to make sure the pets in our care are as comfortable and happy as they can be given the circumstances, so we perform multiple and frequent checks on them during the day, ensuring they are comfortable and free from pain and stress. The checks vary but can be a basic temperature, pulse and respiration (TPR) check for a patient receiving a packed red blood cell transfusion, or for an oxygen dependent patient, or an assessment for analgesia using a pain score chart, or the modified Glasgow coma scale (MGCS) for a neurologically unstable patient. We also administer medications prescribed by the clinicians, this can be either intravenously, intramuscularly, subcutaneously, orally or topically. We are lucky that our Patient Care Assistants are available to take for a walk and feed all of our patients and are very experienced in providing comfort, grooming and encouraging eating. Our physiotherapy team are also on hand to perform physio on our in-patients either in the comfort of their kennel, or in their dedicated physio room.
Here I am spending a little time with a nervous dog, offering reassurance. We have Patient Experience Team who meet regularly and discuss what added value extras, we can provide to make our patients feel happy and relaxed, in this case a pheromone infused soft toy.
During the day as team leaders, we supervise and train the nurses while they are monitoring their patients until they feel confident to perform tasks and observations on their own. So, for example a new RVN to the team would be buddied up with an experienced nurse to gain confidence, while our student nurses are supervised and supported by the whole team while they undergo their training.
We have many different cases that we provide after care for and the day is always very varied. In the photo I am monitoring a patient undergoing a blood transfusion to treat anaemia. I am taking a respiration rate from outside the kennel before taking a heart rate and temperature. We monitor these patients closely for potential transfusion reactions, including TPR and visual observations of their neurological status. This patient is receiving a unit of packed red blood cells which we have purchased from pet blood bank. Pet blood bank come here to collect blood donations a few times a year from fit and healthy dogs that their dedicated owners have given their kind permission for.
As wards team leader I try and catch up with my team every day here is Jenna looking after a very relaxed cat in our dedicated cat ward. This is a cat friendly environment with pheromone diffusers and calm atmosphere, beds and hidey areas in the kennel and covers for the front of the kennels as some cats do prefer to hide.
When we make observations about how our patients are doing we update their hospital notes as we do the rounds during the day. Here I am recording a respiratory rate on a patient form from outside the kennel, before I open the door to perform the heart rate and temperature on a dog recovering from general anaesthesia.
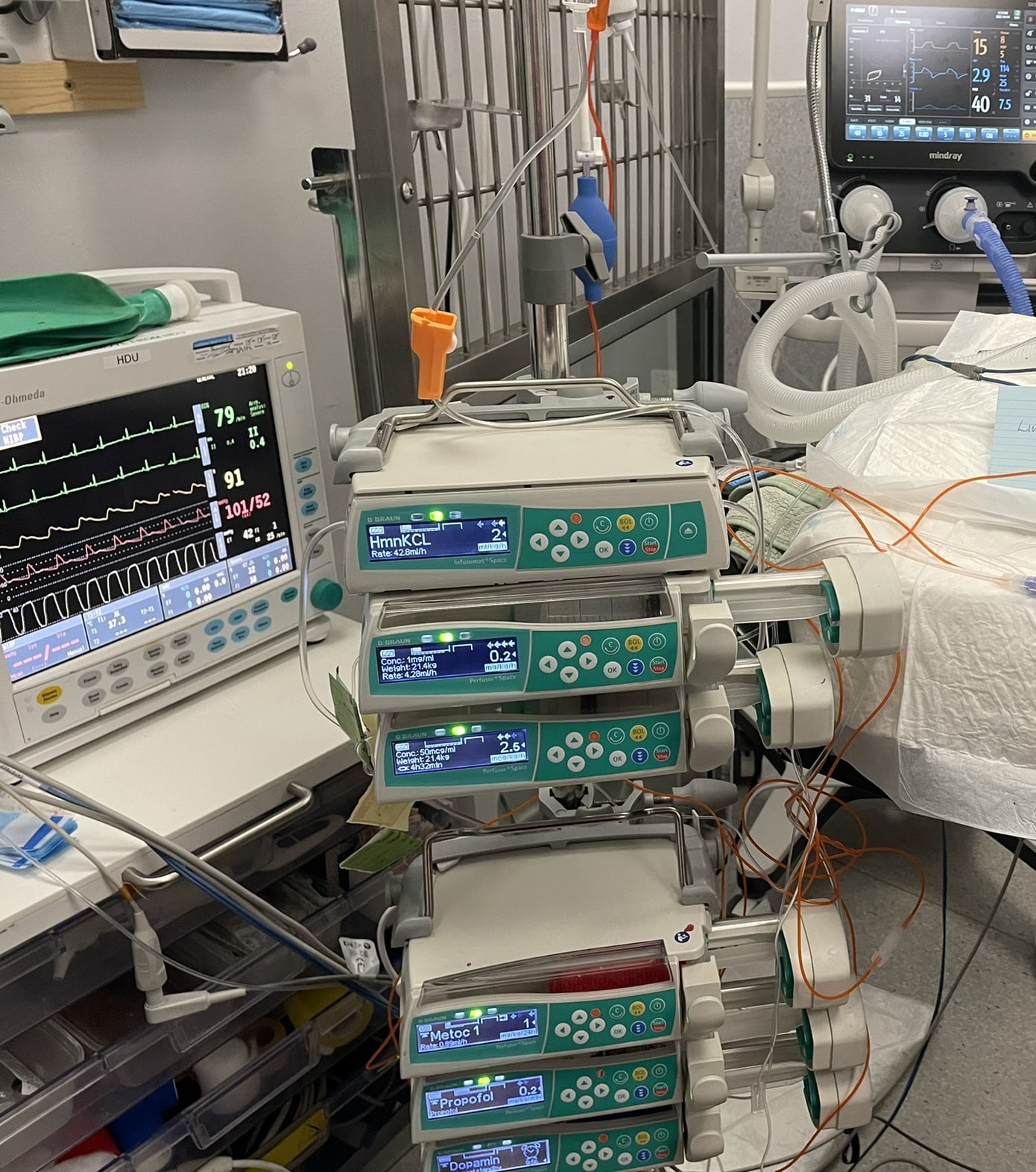
We have an Emergency and Critical Care Service and are pleased to be one of a few facilities south of London offering intensive care unit ventilation and the first to provide ventilation for pets below 5kg. This specialist equipment includes a climate-controlled oxygen cage, high flow nasal oxygen and a paediatric incubator with oxygen monitoring. Here is a cardiac patient being stabilised before having a general anaesthetic for a pacemaker to be fitted.
We are a truly multi-disciplinary hospital so as a nursing team we can be working in the Neurology service one minute, then Orthopaedics and Oncology the next. Here I am taking a tiny dog to the chemotherapy team for vital treatment.
As well as monitoring our patients we do also undertake a number of clinical procedures, taking blood samples, placing intravenous catheters, blood pressure and ECG monitoring. Here I am assisting Leila to take bloods from this patient using his jugular catheter central line.
At the end of the day, we make sure we go through and complete thorough hand-over notes. We handover verbally to the twilight nurses who are taking over the care of our patients. The twilight team will then in turn handover to the night team nurses. The night team nurses will then complete the written handovers ready to hand verbally to the Senior Wards Nurse in the morning. We can use the written handover notes to clarify any points."
Here is a night in the life of one of our night nurses Lindsay Clark RVN GradDipVN VNCertECC
Lindsay qualified as an RVN (Registered Veterinary Nurse) in 2004 and spent time working in primary care before moving to Anderson Moores (AMVS) in 2014. She continued studying and gained her CertVNECC in 2013 and GradDipVN in 2017.
She started at AMVS as a rotating nurse so experiencing all departments within the hospital and settled on internal medicine. She then had children and when she returned to work, she changed to the night shift to give her more flexibility with childcare. She works in the wards overnight but finds the most rewarding work to be in nursing critical care patients in the Intensive Care Unit (ICU).
Here is typical night in ICU;
The night team get a short verbal handover from the day or twilight nurses that have been looking after the patients up until that point. They then take the time to read through the written handover and patient notes from the day to familiarise themselves with the patients, especially if it is their first night overnight.
Patients in the ICU are often really very sick so the team check thoroughly that they have a plan in place and a resuscitation status in case of severe deterioration. The patients could be in ICU for a variety of reasons including that they are on a ventilator; be requiring blood transfusions; be post-surgery so have chest drains or tracheostomy tubes for example; be having seizures; be in respiratory distress so they may need to be on continuous oxygen either via nasal prongs/catheters or in an oxygen kennel; need continuous monitoring for ECG or blood pressure or need to be intensively nursed if they have conditions such as Alabama Rot, Tetanus or Sepsis.
The team then do a series of physical or medical checks on the patients, the situation they are in and the monitoring and checking they require depends on what they are in for. This also gives the team the chance to meet the patients, so they feel comfortable with them.
These checks continue throughout the night, frequently monitoring the patients for any signs of improvement or deterioration – such as their heart rate, respiratory rate, temperature, blood pressure and administering medications. The other checks include placing IV’s; setting up intravenous fluid therapy; taking blood samples; placing urinary catheters, emptying and recording urine output; checking any lines or tubes (central lines, urinary catheters, tracheostomy tubes, feeding tubes) for signs of infection and patency; draining chest tubes and wound drains and monitoring amounts drawn off; placing nasal catheters/prongs and commencing oxygen therapy; respiratory physiotherapy; physiotherapy and recumbency care to prevent bed sores and muscle wastage; using the bedside ultrasound to monitor bladder sizes and if necessary if there is any free fluid in the chest or abdomen that may be of concern; feeding patients by hand or using a feeding tube; walking, bathing and grooming them; if a patient is intubated and on a mechanical ventilator regular suctioning then cleaning their mouth, eye lubrication and cleaning them along with frequent arterial blood sampling to check oxygen levels in the blood. This type of patient requires a nurse to be with them on a 1:1 basis as they need to be continually monitored very closely. And the most important job with all the patients is lots of TLC!
Lindsay said “I write out an hourly med chart, so I know what medications are due and what tasks need to be done to ensure nothing is missed and the pets get the most exceptional care all night. We check medications and do our monitoring routinely at 10pm, midnight and 6am to give the patients time to sleep without being bothered too frequently. In intensive nursing it isn’t always possible, but we do try to give periods of time for rest as it is important for the healing process. We turn the ward lights off at 11pm to help facilitate this. If a patient is on fluids, they would need to go outside more frequently so we also group their walks together with any meds or tasks.
Lindsay continued “Throughout the shift it is important we record notes and make comprehensive observations on the patient’s chart and then towards the end of the shift we write our handover notes which have all the key points about the patient that have occurred overnight before we give our verbal handover to the senior wards nurse in the morning when our shift ends and we go home to get some sleep!”